
What is an Achilles tendon rupture?
The Achilles tendon is one of the largest tendons in the body that connects the calf muscles to the heel bone. It is involved in walking, jumping and running. Two muscles join the Achilles, the gastrocnemius (which goes above the knee) and the soleus (which starts below the knee). A complete rupture is a tear of the tendon in which there is no connection between the two torn tendon ends and the muscles cannot perform their actions.
Who gets an Achilles rupture?
Achilles ruptures can happen in anyone but is commoner in men and typically happens between the ages of 30-50. Other risk factors that weaken the tendon include; those with an abnormal tendon (tendinopathy); certain medication like steroids or certain antibiotics (fluoroquinolones); and those who have had a steroid injection into the tendon.
What are the symptoms of an Achilles rupture?
Patients often experience a sudden pain like they have been hit directly into the back of the heel. They may even hear a snap. It is not uncommon for them to turn around and blame someone close for hitting them, even though they did not! Pain is variable and some patients are in severe pain, others no pain at all. Some patients might not be able to walk properly.
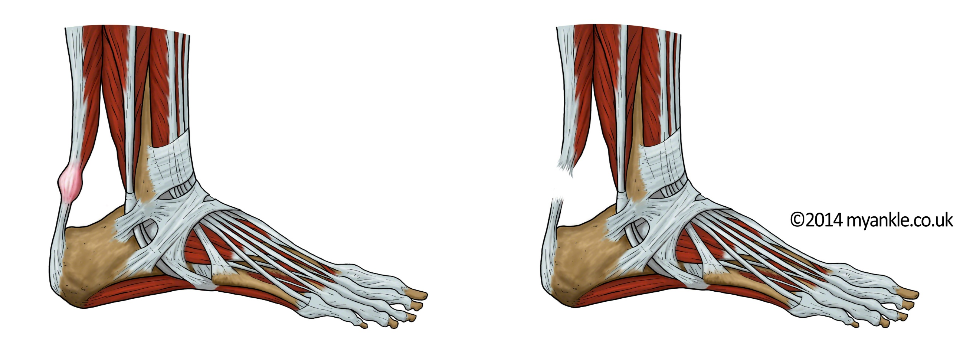
Acute Achilles tendon rupture
How is an Achilles rupture diagnosed?
To diagnose a rupture, a health professional would usually ask the patient to lie on a bed or couch, turn onto their front lying with both feet hanging off the end of the couch. There are three cardinal clinical signs of an Achilles tendon rupture:
1. The first sign is that the affected foot hangs at a different angle than the unaffected side. This is known as an increased angle of dangle, so that the toes are closer to the bed than the other side. This is because a normal muscle has tone, which is lost following tendon rupture as the muscle is no longer connected. An increased hanging angle implies that the tendon ends are separated.
2. There may be a gap felt between the two tendon ends and your specialist can put a finger into the gap. This is not always the case, if presentation is delayed and the gap is filled with clotted blood and scar tissue.
3. If the examiner squeezes the calf muscles on the normal side the toes should flex down. On the affected side no motion of the toes happens when the calf is squeezed because the muscle is no longer connected to the tendon. This is known as a negative squeeze test.
If all three cardinal signs are present, then a complete tendon rupture can be diagnosed. In some circumstances only one or two of these signs are present. An ultrasound scan will usually be required, not just to confirm the rupture which is obvious, but to provide essential information to help your specialist know how best to manage the rupture. This includes the quality of underlying tendon (is there tendinopathy or tendinitis?); and does the gap close by bringing the foot and toes into a high heel position?
How is Achilles rupture treated?
Treatment involves holding the toes away from the body (a high heel position) so that the tendon ends can come together or overlap and then holding them there to repair. The repair can take 12 weeks to become strong but the remodeling of the tendon may take up to 12-24 months. The first 6-8 weeks of the healing is a crucial phase and the foot needs to be held in a downwards (equinus) position to allow them to join up. This position can be held in a plaster of Paris cast or in a special walker boot which has a hinge, known as a VACOped® Boot. If the two tendon ends are not opposed, then the tendon is still likely to heal but it will usually heal stretched or with partial scar tissue. This can lead to weakness and carries an increased risk of re-rupture.
There are many studies comparing surgery to repair the tendon against non-surgical treatment and the best of these studies show that if the tendon ends are opposed then the outcome is most likely to be the same with or without surgery. If the ultrasound scan shows that the tendon ends cannot be brought together even with the toes pointing downwards then your specialist may recommend surgery to improve the chances of a better outcome.
Irrespective of surgery or no surgery, in the first few days it is essential that to elevate the ankle to keep the swelling down. Patients are placed into a plaster cast or a VACOped® walker boot and to use crutches and should put no weight through the affected foot until advised by your specialist. Usually, this is for the first two to three weeks in order for the initial repair to take place. After that point, load can help stimulate tendon healing and encourage the muscle to stay healthy. Your specialist will then gradually bring the foot up to neutral (flat to the floor) over a 10-12 week period.
Pros of non-operative treatment
The pros of non operative treatment include no risk of a surgical complication (from the anaesthetic or the surgery itself). Note that certain risk factors increase the chances of surgical complications and may be a reason to recommend non-surgical treatment. These include: smoking; age above 60; delayed presentation (more than 10 days); and conditions like diabetes, or the use of medication, such as steroids.
Cons of non-operative treatment
There are of course some downsides to non-surgical treatment. These include an increased risk of re-rupture. This one is not strictly a re-rupture, but more likely a tear through the healing scar tissue which has not yet turned into tendon. If the tendon ends heal stretched, then there may be some weakness of push off, especially single leg heel raises. Finally, your therapist will need to be slightly slower with your rehabilitation programme to avoid the rupture or lengthening described above.
Surgery for Achilles tendon rupture
If your surgeon recommends surgery, this is usually because they consider that non-operative management is likely to have a poorer outcome. The reasons for this are usually that the two tendon ends do not oppose and there is a sizeable gap between them. Re-ruptures of tendons also tend to be treated with surgery.
Most surgeons use an open technique because the incidence of nerve injury is high and too unpredictable with some of the various percutaneous (or minimally invasive) treatments available. With open surgery the incision is very small, and the sural nerve can be identified and protected. As with all surgery there are risks and it important that you discuss these with your surgeon before proceeding.
Frequently Asked Questions about Achilles Rupture
When can I drive after an Achilles tendon rupture?
Driving is allowed once you are safe to do an emergency stop. For most patients that rupture their left Achilles, they usually can drive an automatic car after 2 weeks. If you rupture your right Achilles then it is more likely going to take 3-4 months before you can safely drive again.
Am I at risk of a blood clot?
A ruptured Achilles increases your risk of a clot in your calf (deep vein thrombosis). This is because of swelling and lack of muscle activity, and the risk is present whether you are treated with or without surgery. To reduce this risk, The National Institute of Health & Care Excellent (NICE) Guidance recommends that doctors discuss with you the use of blood thinners for about 28 days.
How long does it take for the tendon to heal?
When the tendon tears, it bleeds into the gap between the shredded tendon ends. The blood contains stem cells which are the body’s healing cells. These cells can become tendon cells, scar tissue, or bone. It’s important that whilst this healing is taking place that the repair tissue is not overstretched as this can lead to the formation of poor quality tendon, scar tissue or even bone. Initial tendon healing takes 10-12 weeks, but the full remodelling of the tendon takes up to 24 months, during which time neuromuscular retraining is key to rehabilitation. This is where the muscle and tendon are trained to work together harmoniously.
This article was written by Mr Andrew Goldberg, a Consultant Orthopaedic Foot & Ankle Surgeon in London. Mr Goldberg uses an accelerated rehabilitation programme for Achilles Ruptures that aims to get patients back to their optimum performance in the shortest possible time. To arrange an out patient appointment with Mr Goldberg please contact +44(0)207 042 1828 or email [email protected]
