Ankle fusion, also known as arthrodesis, is a surgical procedure that is often recommended for patients suffering from severe arthritis or other debilitating conditions in the ankle joint. This procedure aims to alleviate pain and improve stability by fusing the bones of the ankle together, eliminating the joint entirely. Here’s what you need to know about ankle fusion, its benefits, and what to expect.
Understanding Ankle Fusion
The ankle joint is a complex structure that connects the bones of the lower leg (tibia and fibula) to the foot (talus and tarsal bones). In a healthy ankle, these bones are separated by the shock-absorbing articular cartilage, which acts as a cushion and allows for smooth movement. However, conditions like arthritis, trauma, or deformities can damage the cartilage, meaning bones can rub against bones, leading to pain, swelling, and stiffness.
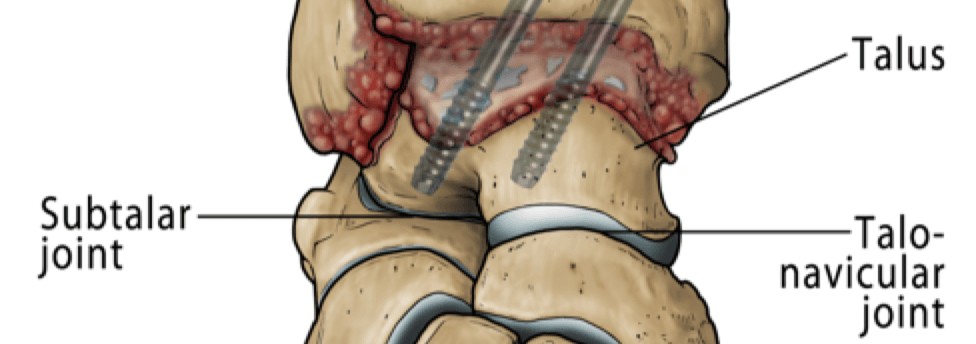
Ankle fusion involves surgically removing the damaged cartilage and fusing the bones together with screws, plates, or rods. This creates a single bone, preventing any movement between them. While this might sound limiting, the goal of the surgery is to relieve chronic pain and improve the patient’s quality of life by providing a stable and pain-free ankle. Because the foot has 30 joints you may be surprised at how much mobility remains after the ankle joint is stiffened.
Who Needs Ankle Fusion?
Ankle fusion is typically considered when other treatments have failed to relieve symptoms. These treatments might include medications, physical therapy, or less invasive surgeries. Conditions that often lead to the need for ankle fusion include:
- Primary osteoarthritis: Wear and tear of the articular cartilage, often in your 50’s or 60’s and runs in families.
- Rheumatoid or Inflammatory arthritis: An autoimmune or metabolic condition that attacks the joints.
- Post-traumatic Arthritis: osteoarthritis that develops after an injury. This is the commonest type affecting the ankle.
- Severe Ankle Deformities: Such as those caused by recurrent sprains, neuromuscular diseases or congenital deformities.
What Is Ankle Fusion Surgery?
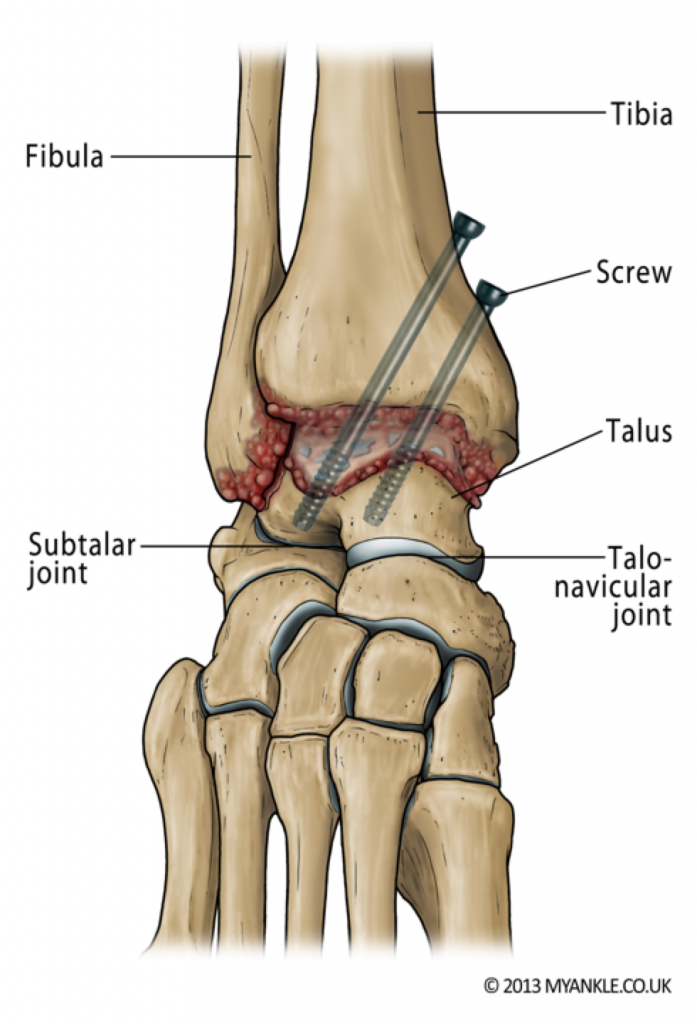
Ankle arthrodesis (ankle fusion) is an operation to “fuse” or stiffen the ankle joint. Ankle fusion surgery involves removing the surfaces of the damaged ankle joint and fusing the tibia to the talus bone, so that your foot is under your body and flat to the floor.
This procedure can be performed as keyhole surgery (also referred to as arthroscopic surgery) or open surgery. In keyhole surgery, a number of small incisions are made. Whereas in open surgery, a larger incision is made. The damaged joint surfaces are removed and the bones are held together using screws to maintain the position while bone healing occurs and the bones “fuse” together to become one. This converts a stiff, painful joint into a stiff but pain-free one.
The surgery takes between one and two hours. You will have a tourniquet applied around your thigh during the surgery, to reduce bleeding.
What Happens Following Ankle Fusion Surgery?
When you wake from surgery you will have a below-knee partial cast. Which may later be changed into a full below-knee plaster or synthetic cast. You will have to wear a cast for up to 12 weeks. You will need crutches or a frame to help you move around during this time.
Depending on your situation, your surgeon will allow you to weight bear after 6 weeks and sometimes sooner. You should discuss your post-operative care with your surgeon.
Because you are immobilised after surgery, it is usually recommended that you have blood-thinning medication to prevent blood clots whilst in the cast. As well as a special stocking on the other leg to improve blood flow.
After the plaster cast is removed, you may require an ankle brace or a walking boot for a few more weeks. You will then be able to wear your normal shoes. Sometimes changes are made to the sole of the shoe to give you a normal stride length despite the stiffened joint.
In some circumstances where there is a major deformity or where the arthritis affects more than one joint, your surgeon may recommend fusion of more than one joint. There are lots of surgical options including a tibiotalocalcaneal fusion or a pantalar fusion. These may involve a rod or a large metal nail inserted up to the middle of the shinbone through the heel. To find out more please visit the ankle arthritis TARVA Website.
What Can I Expect After Ankle Fusion Surgery?
Ankle arthrodesis provides excellent-pain relief and good function. It has a 90% success rate, as measured by patient satisfaction in the short to medium term.
Some patients express concerns regarding the level of mobility they will have following surgery. Ankle fusion surgery removes ankle movement completely; however, because there are 30 joints in the foot, as much as 50% of the up and down movement of the foot can be maintained. It is important that you have an MRI scan or an alternative type of 3D imaging before undergoing surgery, as it is essential to document the health of the adjacent joints before you have one joint fused.
Walking
In most cases, walking will return towards normal, so that others may not notice that you have had an ankle fusion surgery. If you walked with a limp prior to surgery because of pain, after the surgery your walking is likely to improve. Because the stride length is shorter, a limp may be noticeable if you start to run. Some female patients comment that it is uncomfortable or not possible to wear high-heeled shoes after ankle arthrodesis.
Sports
Most patients with a successful ankle fusion surgery are able to walk without a limp, cycle and do certain sports such as golf. Although more vigorous activities such as squash, tennis or football may be possible after an ankle arthrodesis, we do not recommend them. This is because contact sports put a lot of stress across the adjacent joints, which will wear with time, and pain may return. Similarly, walking or hiking on rough ground is possible but will put more stress on the adjacent joints. You can protect the adjacent joints by wearing a sturdy above-ankle walking boot.
Ankle Fusion Surgery – Post Op
This video shows a 42-year-old man 1-year post arthroscopic ankle fusion surgery. He is able to stand on his tiptoes and jog, albeit with a slight limp.
Are there any major risks with ankle fusion surgery?
In addition to the general risks of ankle surgery, the specific risks of ankle arthrodesis relate to problems with union and transference of stress to the adjacent joints.
- Non-Union: Research has shown that about 11% of fusions do not fully heal after surgery and a visible line shows on the X-rays after 1 year. Not all patients have symptoms however. About 8% of patients do have symptoms enough to warrant a second operation to redo the fusion. If you smoke, your risk of such a complication is greatly increased. You will be advised to stop smoking before surgery.
- Adjacent Joint Arthritis: Because the ankle joint has been stiffened, more stresses will be taken by adjacent joints, which, with time, are at risk of wearing. Signs of arthritis in the adjacent joints are common on X-rays after 10 years, but many patients do not require treatment for this.
- Need for Further Surgery: Sometimes the screws become prominent under the skin. If this happens, they can be removed but only about 1 in 10 patients need the screws to be taken out. If screws need removing, we usually advise you to wait at least a year after surgery to give the bones time to become strong.
General complications following ankle fusion surgery:
Swelling
You should expect some swelling for up to one year after surgery. Elevation of the limb above heart level for the first two weeks helps to reduce swelling and aid wound healing. If swelling persists and you are concerned, seek medical advice.
Bleeding
All wounds bleed after surgery, but rarely this can be excessive causing wound problems or requiring further surgery.
Painful scar
Any type of surgery will leave a scar. Some people develop larger scars than others. Occasionally this can cause pain and irritation. If you suspect you are prone to scar problems please discuss this with your surgeon prior to surgery.
Infection
Superficial wound infection (redness around the wound) occurs in up to 5% of cases. Much rarer (less than 1%) is a deep infection where the metalwork or bone is infected. Minor infections usually clear up with a course of antibiotics. More serious infections may require further surgery and involve complex and lengthy treatment.
Nerve injury
Numbness or tingling at the surgical site is common and is usually temporary. However, up to 50% of patients who have an open ankle fusion surgery will get some numbness on the top of their foot. This is not usually a problem. If a key nerve is injured (up to 1.5% of cases) then it can cause permanent numbness and shooting pains requiring medication or further specialist input. Rarely the sympathetic nerves (also known as fight or flight nerves) react badly after the surgery, and cause temperature and colour changes to the skin – this is known as complex regional pain syndrome (less than 3%) and can take up to 12-18 months to settle. Occasionally it does not settle and causes long term pain.
Blood clots
Deep vein thrombosis (DVT) is uncommon (5%), and pulmonary embolus (PE) is very rare (less than 0.5%) and occurs due to blood clots. We do everything to minimise these risks but they can occur and can be serious causing prolonged leg swelling or chest problems. Blood-thinning medication may be given to prevent blood clots whilst in a cast as well as a special stocking on the other leg to improve venous circulation.
Audit & Research
The two main treatments for ankle arthritis are ankle fusion and ankle replacement.
There is a randomised controlled trial comparing ankle replacement against ankle fusion (TARVA) – see http://clinicaltrials.gov/ct2/show/NCT01518361.
Click here to find out about ankle replacement