Tendinopathy describes an unhappy tendon. There is a lot of confusion between the terms tendinitis, tendinopathy, tendonopathy, and tendinosis. Generally, the terms can be used interchangeably. However, the agreed term nowadays is tendinopathy as a catch-all.
Achilles Tendinopathy
A tendon connects a muscle to a bone. Think of a tendon as being a million small elastic bands. Each one is stretchy, returning to its normal shape after being stretched. If you stretch an elastic band beyond its elastic limit then it no longer behaves like an elastic band and is useless.
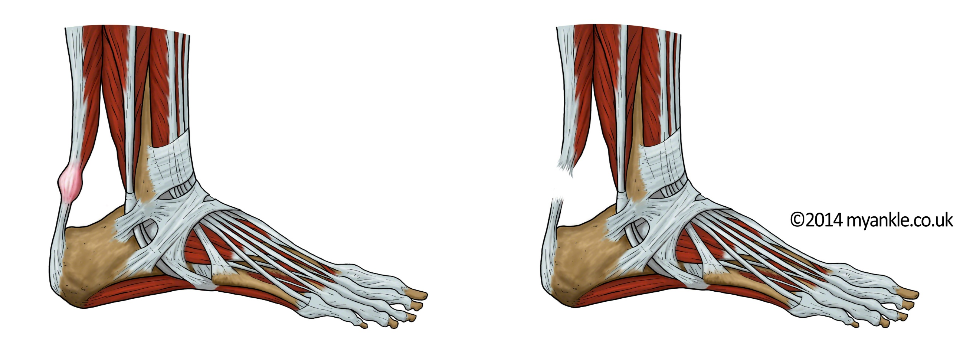
This is a good way to think about achilles tendinopathy. A few of the fibres of the tendon are damaged from being overstretched. As a result, in the initial stages, the body responds with inflammation and swelling and tenderness. After a while, the tendon fibrils themselves become degenerate. Leaving an area of damaged unhealthy tendon within the surrounding healthy fibres. This is chronic tendinopathy.
The Achilles is the biggest tendon in the body. It is responsible for running, hopping and jumping and commonly suffers from tendinopathy.
How common is Achilles Tendinopathy?
About 80,000 people a year seek their doctors’ advice for Achilles tendon pain each year in the UK and perhaps 5 times this amount in the USA. It commonly affects joggers and runners. Who have a lifetime risk of 1 in 2 or 50% to develop Achilles Tendinopathy problems. In addition, it also affects athletes who play almost any sport. This includes tennis, football, volleyball, badminton, or squash. On the other hand, it can also affect the non-active or weekend warriors.
Who is at risk of developing Achilles Tendinopathy problems?
Aside from the sports mentioned above, typically Achilles tendinopathy problems can affect runners in the 30’s and 40’s but any age is possible. Being overweight is a risk factor, as well as being male. In addition, other risk factors include poor training techniques, diabetes, stiff joints, and weak. As well as being generally deconditioned.
How to treat Achilles Tendinopathy?
The main treatment is physiotherapy. A good therapist will take a thorough clinical history and learn about your training patterns. Specifically, they will look for things that are risk factors. For example; alignment issues, generalised weakness and poor training patters where they will try and help address these.
Neuromuscular rehabilitation is the mainstay of treatment. This includes exercises that retrain the brain, muscles and nerves to work better. Although they are not always eccentric, quite often these exercises are called eccentric exercises. Consequently, the neuromuscular rehabilitation is much more important. Your physiotherapist will support you with a program by seeing you on a regular basis.
What if my Achilles tendon pain is not improving?
If your Achilles tendinopathy pain is not improving despite good physiotherapy treatment its important to seek an expert opinion. Firstly to confirm that the diagnosis is correct. This is because sometimes pain coming from the back of the ankle or leg or referred pain from higher up can present with heel pain. Moreover, its also important because there are other treatments now available.
Is there any research into Achilles tendinopathy?
There is a lot of active research into Achilles tendinopathy. An example is a first in man study looking into the use of the patients own stem cells to treat their Achilles. A study funded by the UK Stem Cell Foundation, called ASCAT, is in the process of being published.
Did you enjoy this article? You may also like; How to find London’s best ankle surgeon